Viruses to Cure Cancer
Optimal cancer therapy leading to a cure has not been achieved in all tumour types. The best strategies for new treatment remain to be defined, but we need to look beyond traditional chemotherapy and radiotherapy.
Our laboratory has an interest in so called “oncolytic viruses” or cancer killing viruses. The idea behind the concept of oncolytic viruses is best illustrated by the case of an 8 year old boy with Burkitt’s Lymphoma (solid tumour). He became infected with measles virus, after which the tumour went away. This case shows us that oncolytic viruses are able to grow in and kill tumours. More recently it has been shown that the way in which the virus kills the tumour cells is also important. The virus kills the tumour cell in such a way that it kick starts the immune system into mounting an immune response against the tumour. Thus oncolytic viruses have a two pronged approach to cancer killing both directly via infection and lysis and indirectly using the body’s own immune system.
Oncolytic Viruses
Dr Guy Simpson is an expert in oncolytic viruses. In the past he developed a herpes simplex virus that has now gone through all three phases of clinical trials becoming, this year, the first so called “ oncolytic virus “ or cancer killing viruses to show efficacy in patients. Both herpes simplex virus (HSV) and reovirus are able to replicate within tumour cells and not in normal healthy cells of the body due to a specific mutation of a gene common to many cancers. As the virus replicates within the tumour cells new viral offspring are produced. These burst out of the cell causing the tumour cell to pop and die.
Recently Guy worked on a novel cold related virus called Coxsackie virus which is currently in phase I-II clinical trials for melanoma (skin cancer). His preliminary experiments have shown that by incorporating the section of bacterial protein the ability of the virus to stimulate the immune system is boosted significantly. After studying the virus in bladder cancer, it was shown that:
Results of Our Studies
We have recently published these results: ‘Oncolytic Immunotherapy for Bladder Cancer Using Coxsackie A21 Virus’. Nicola E. Annels, Mehreen Arif, Guy R. Simpson, Mick Denyer, Carla Moller-Levet, David Mansfield Rachel Butler, Darren Shafren, Gough Au, Margaret Knowles, Kevin Harrington, Richard Vile, Alan Melcher, Hardev Pandha.Molecular Therapy Oncolytics. Volume 9, p1–12, 29 June 2018
The preliminary work from these in vitro laboratory studies has allowed us to conduct a phase I first in man clinical trial using the Coxsackie virus in non-muscle invasive bladder cancer. The results of the trial were positive and showed an acceptable safety profile for the Coxsackie Virus (CAVATAK) (no grade 2 or higher adverse events), proof of concept of viral targeting, replication and tumour cell death together with virus-mediated increases in immune response within the tumour microenvironment. This indicates that this oncolytic agent is likely to signal a strong local and systemic anti-tumour immune response. We are soon to publish this data in a high impact journal ‘Phase I/II CANON study: Oncolytic immunotherapy for Non-Muscle Invasive Bladder Cancer (NMIBC) using Intravesical Coxsackievirus A21’. N. E. Annels1, D. Mansfield2, M. Arif1, C. Ballesteros-Merino3, G. Simpson1, S.S. Sandhu4, A. A. Melcher2, K.J. Harrington2, B. Davies4, G. Au4, M. Grose4, I.Bagwan1, B.A. Fox3, Richard Vile5, H. Mostafid1, D. Shafren4, H.S. Pandha1*.
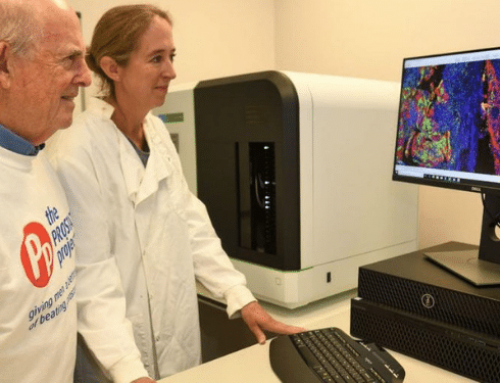
The Prostate Project funded a PhD student Mehreen Arif for 3 years. Mehreen contributed significantly to the coxsackie virus work and has recently submitted her thesis. She is now working at Glaxo Smithkline as a postdoctoral fellow.
Strain of Common Cold Virus Could Revolutionise Treatment of Bladder Cancer
How Can a Strain of Common Flu Help?
A strain of the common cold virus can infect and kill bladder cancer cells, a small study in the Clinical Cancer Research journal reports. All signs of the disease disappeared in one patient, and in 14 others there was evidence that cancer cells had died.
Our cancer research team at University of Surrey said the virus could “help revolutionise treatment” for the cancer and reduce the risk of it recurring.
Non-muscle invasive bladder is the 10th most common cancer in the UK, with around 10,000 new cases each year. Bladder cancer costs the NHS more per patient than nearly every other cancer, because of the high recurrence rate
Current treatments for this type of bladder cancer are invasive or can cause serious, toxic side effects. And constant, costly monitoring is needed to check that the cancer has not returned after treatment.
‘Join the Party’
In this study, 15 patients with the disease were given the cancer-killing coxsackievirus (CVA21) through a catheter one week before surgery to remove their tumours. When tissues samples were analysed after surgery, there were signs the virus had targeted and killed cancer cells in the bladder. Once these cells had died, the virus had then reproduced and infected other cancerous cells – but all other healthy cells were left intact.
What the virus does is special, says study leader Prof Hardev Pandha, from the University of Surrey and Royal Surrey County Hospital.
“The virus gets inside cancer cells and kills them by triggering an immune protein – and that leads to signalling of other immune cells to come and join the party,” he said. Normally, the tumours in the bladder are “cold” because they do not have immune cells to fight off the cancer. But the actions of the virus turn them “hot”, making the body’s immune system react.
Prof Pandha said the same virus had also been tested on skin cancer, but this was the first time it had been studied in a clinical trial on bladder cancer.
“Reduction of tumour burden and increased cancer cell death was observed in all patients, and removed all trace of the disease in one patient following just one week of treatment, showing its potential effectiveness,” he said. “Notably, no significant side effects were observed in any patient.”
A New Era in Treatment
The plan is now to use the common cold virus with a targeted immunotherapy drug treatment, called a checkpoint inhibitor, in a future trial in more patients.
Dr Nicola Annels, research fellow at the University of Surrey, said viruses like the coxsackievirus “could signal a move away from more established treatments such as chemotherapy”.
Dr Mark Linch, a bladder cancer expert at the Cancer Research UK Cancer Institute at University College London, said the initial results were “encouraging”.
“It will be really interesting to see how this new virus-based therapy fares in larger trials in people with non-muscle invasive bladder cancer, particularly in combination with newer immunotherapies,” he said.